A years-long investigation into a home health care provider in Highland, Indiana, has resulted in a $217,000 settlement and criminal conviction obtained through the hard work of Attorney General Todd Rokita’s Medicaid Fraud Control Unit (MFCU).
Following a tip, MFCU investigators discovered that Allpoints Home Health Care Inc. billed the Medicaid program for thousands of hours not actually worked. In all, the business was found to have submitted 1,055 false claims.
“Week after week, our nationally renowned Medicaid Fraud Control Unit does outstanding and incredibly thorough work on behalf of Hoosiers,” Attorney General Rokita said. “And of all the types of fraud committed, what is more sinister than stealing money which was intended to help low-income sick people pay their health care bills?”
In some instances, the perpetrators were particularly sloppy in their falsification of records — such as claiming to provide home health care to one patient during a time when that individual was hospitalized and not even at home to receive the purported home services.
As part of the investigation, MFCU staff analyzed claims submitted to Medicaid, interviewed Allpoints employees, reviewed medical records and perused Electronic Visit Verification sheets.
By the time all the facts were gathered, investigators had enough evidence not only to pursue a settlement but also to work with the Lake County Prosecutor’s Office to achieve a criminal conviction as well.
Mohammad Adnan Satti — the employee who prepared and submitted the majority of the false claims — was convicted for felony theft and sentenced to 18 months suspended jail time as part of a plea agreement.
Allpoints agreed to pay Indiana $217,019.61 in exchange for escaping civil liability for violations of the Indiana Medicaid False Claims and Whistleblower Protection Act. That’s three times the overpayments identified by our team’s analysis of the claims data.
Attorney General Rokita thanked MFCU Director Matt Whitmire, Deputy Attorney General Jeremy Johnson and former Deputy Attorney General Jordan Stover for their work on this case.
The Indiana Medicaid Fraud Control Unit receives 75 percent of its funding from the U.S. Department of Health and Human Services under a federal grant. The remaining 25 percent is funded by the State of Indiana.

 Gov. Mike Braun orders flags to half-staff for Pearl Harbor Remembrance Day
Gov. Mike Braun orders flags to half-staff for Pearl Harbor Remembrance Day
 Stay safe; always assume you are on ‘thin ice’
Stay safe; always assume you are on ‘thin ice’
 100% of Keystone Cooperative member profits returned to farmer-members
100% of Keystone Cooperative member profits returned to farmer-members
 More than $320,000 in energy bill assistance available for Duke Energy Indiana customers
More than $320,000 in energy bill assistance available for Duke Energy Indiana customers
 Niles Scream Park raises more than $153,300 for local groups
Niles Scream Park raises more than $153,300 for local groups
 Indiana Senate accepting applications for 2026 Page Program
Indiana Senate accepting applications for 2026 Page Program
 Indiana Farm Bureau Insurance surpasses 2024 volunteer impact, continues Giving Tuesday initiative
Indiana Farm Bureau Insurance surpasses 2024 volunteer impact, continues Giving Tuesday initiative
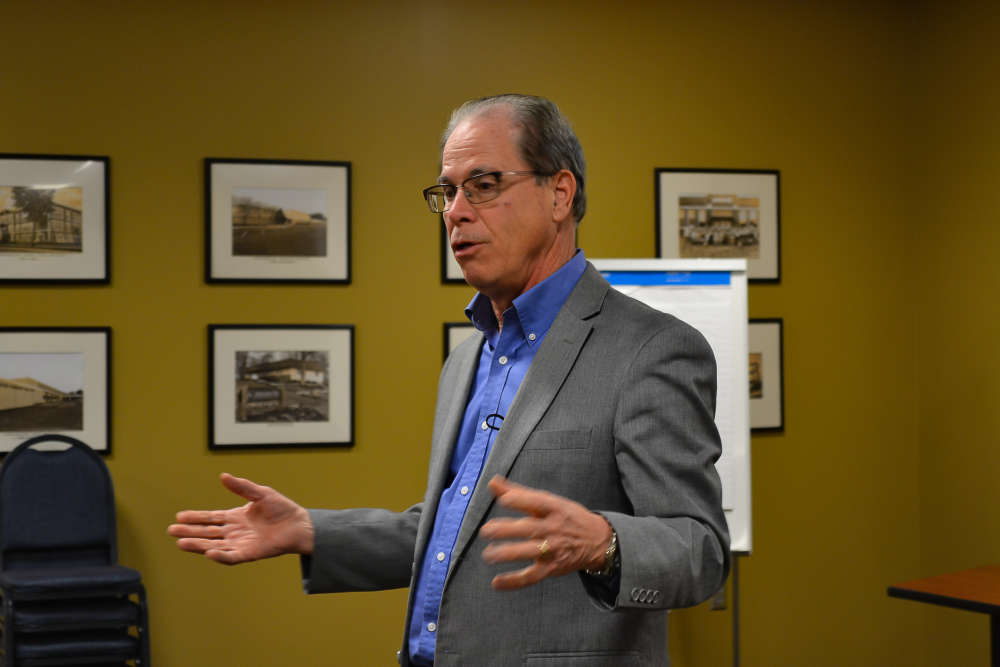 Governor Braun announces "Family First Workplace” policy to support working families
Governor Braun announces "Family First Workplace” policy to support working families
 Two nabbed for drugs in Parke County
Two nabbed for drugs in Parke County
 USPS asks public to clear snow and ice to help deliveries
USPS asks public to clear snow and ice to help deliveries
 Winter Weather Advisory calls for more snow chances
Winter Weather Advisory calls for more snow chances
 Special Olympics Indiana now serves 20,000 athletes statewide
Special Olympics Indiana now serves 20,000 athletes statewide
 Winter Storm Watch for most of central Indiana, heavy snow possible
Winter Storm Watch for most of central Indiana, heavy snow possible
 Dana Festival of Lights right around the corner
Dana Festival of Lights right around the corner
 Governor Braun celebrates "Small Business Saturday" in Indiana
Governor Braun celebrates "Small Business Saturday" in Indiana
 New Coach Curt Cignetti Indiana Hoosiers bobblehead unveiled with proceeds going to Riley Children’s Hospital
New Coach Curt Cignetti Indiana Hoosiers bobblehead unveiled with proceeds going to Riley Children’s Hospital
 IDOH offers food preparation tips for a safe Thanksgiving
IDOH offers food preparation tips for a safe Thanksgiving
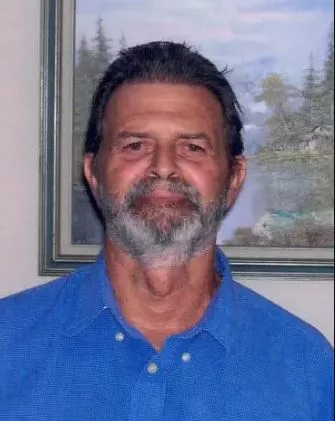
 O'Heir reflects back on time as Vermillion County EMA Director
O'Heir reflects back on time as Vermillion County EMA Director